Our comprehensive fertility testing guides our doctors to develop a plan unique to your infertility history and situation to help you achieve your dream of having a family. As a low-cost fertility center, we focus on doing the testing that you need to make a diagnosis to keep the cost of your fertility journey as low as possible.
At a Glance
- Only the testing you need
- Both partners will undergo testing
- Blood test and imaging are commonly performed
- AMH to measure ovarian reserve
- Tubal or uterine testing via HSG or FemVue
Female Fertility Testing
Our providers at Pathways Fertility have over 60 years of combined experience in helping families in Atlanta and across the country to bring healthy babies into the world. Unfortunately, getting pregnant and having a child does not come easily for everyone. It is recommended that a woman seek help from an infertility specialist if she has been trying to conceive for over one year, or if she is over age 35, if she has been trying for 6 months.
Approach
Both the man and the woman undergo fertility testing to some degree, even if there is a known fertility issue to be addressed. The first step of the male fertility evaluation is simple. If a semen analysis verifies that the quality of the spermatozoa is normal, then the focus is on the female. If the semen is not normal, further male testing is needed.
Blood Testing
A series of blood tests and imaging tests are involved in testing women who have been trying to conceive. Below are some of the female infertility testing that may be done in a step-wise fashion depending on your history of trying to conceive.
Ovarian Reserve Testing
The anti-mullerian hormone (AMH) test, available through your doctor’s office, helps to determine your ovarian reserve which reveals the potential supply of eggs. This sophisticated test requires an outside lab which returns the results within a week. A high result means that a woman has a high probability of getting pregnant. Although if it is a very high result, she may have polycystic ovarian syndrome. If the result is below average, this means that she may have a lower chance of conceiving naturally. The normal range is between 1.0 to 4.0 ng/mL.
What is the ovarian assessment report (OAR)?
The ovarian assessment report (OAR) is a patented algorithm of tests which uses a single blood sample for assessing the ovulatory egg supply in women. A test called Inhibin B is an indirect measurement of the supply of eggs. FSH, the hormone produced by the pituitary, is used along with the reliable AMH test. A specific mathematical formula provides predictive power of all of these hormones by providing an “egg retrieval score” which predicts the number of eggs that might be obtained after ovarian stimulation for IVF as well as the chances of having good quality eggs. The score, comparing a specific patient to over 1,000 women treated at fertility centers, is rated good, average or reduced for the particular age of a patient who is having her ovarian reserve estimated. As a practical matter, the AMH test by itself is commonly used by physicians in reproductive endocrinology in order to predict the outcome. We do not request the OAR often because of its cost.
THS Test
The thyroid stimulating hormone test is performed on all women who have been trying to conceive for over one year and are investigating their fertility. It is very common for women to have elevated TSH levels which indicates hypothyroidism, a slightly underactive thyroid condition. It is uncommon to find low TSH, indicating thyroid over function (hyperthyroid). It is also uncommon for the thyroid to be so out of balance that it causes infertility. Extreme instances of thyroid problems can cause lack of ovulation. In these cases, the periods would stop or be irregular. For reproductive purposes, a cut-off level of TSH around 2.5 mIU/mL is considered an ideal strict criterion. Reproductive endocrinologists encourage patients whose TSH is above this level to consider taking thyroid hormone. If they are not trying to conceive, mild TSH elevation is not as important. Other thyroid tests for T3 and T4 are only checked if TSH is elevated since these antibodies are not a cause of reproductive failure if the thyroid hormone levels are normal. Thyroid antibodies may be positive, indicating an autoimmune cause for subclinical hypothyroidism.
Prolactin Hormone
Particularly in women who have irregular periods (amenorrhea), and noted nipple discharge, the prolactin hormone will be tested. Severely elevated prolactin hormone can cause anovulation where no egg is released during the menstrual cycle, amenorrhea or stopping periods. This can be due to a tiny benign pituitary tumor and can be treated with medication. Unless the patient has irregular periods, prolactin elevations are usually not the cause of the infertility, but still should be managed appropriately.
Imaging Tests
There are a number of specific imaging studies, each with a different objective, that are useful in understanding the cause of infertility.
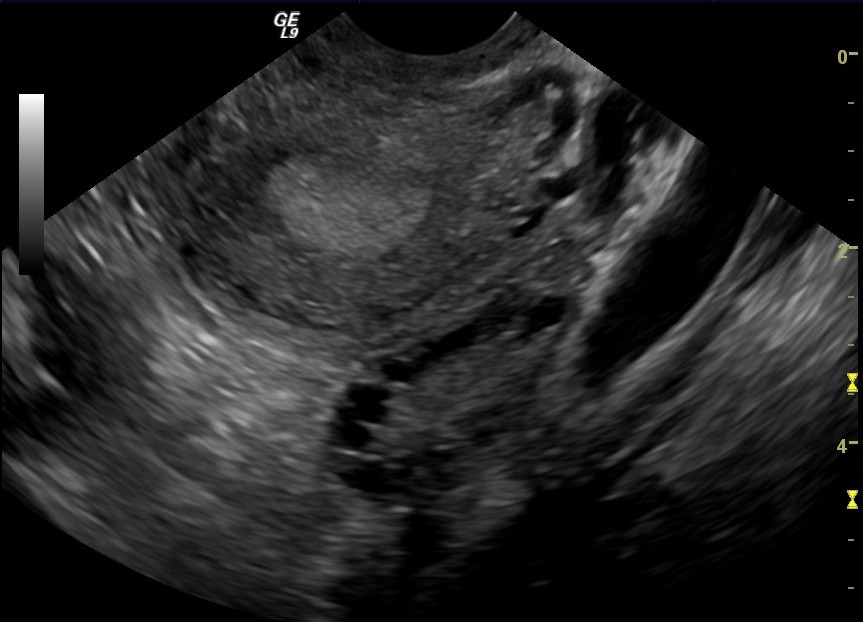
Pelvic Ultrasound
At the first visit to an infertility specialist, a pelvic ultrasound is performed. Most commonly done transvaginally, the ultrasound probe produces high-frequency sound waves allowing visualization of the uterus and ovaries. The tubes cannot be seen. Common observations include measuring the size of the ovaries and checking for cysts. Certain types of cysts can be seen, which have a ground-glass appearance and are typical of severe endometriosis. Under ultrasound, fibroid tumors can be observed, which need to be evaluated for placement and size.
Basal Antral Follicle (BAF) Count
Most patients have small follicles in the ovary called antral follicles which develop eggs for ovulation within the next two or three months. The antral follicles are counted and measured with ultrasound. The higher the number of antral follicles, which are 10mm or less in size, the better. It is a good predictor of the number of eggs found at retrieval for IVF. For example, a typical patient in her mid 30s may have five antral follicles on each ovary. Sometimes patients have over 12 on each side; this is characteristic of polycystic ovaries which can be associated with infertility. Low numbers can be associated with low or diminished ovarian reserve. Sometimes the BAF is more predictive than AMH.
Sonohysterogram (SIS)
The sonohysterogram (SIS) is a method to examine the lining of the uterus and determine if it is free of polyps and fibroids. During this procedure, saline solution is placed into the uterus with a small catheter. A balloon is used to provide a seal for better distention of the uterus. The SIS provides a clear picture of the lining of the uterus. Polyps can be detected, which can be removed later. Fibroids, which might interfere with fertility, can be assessed as well. Both the saltwater and the balloon may cause some mild to moderate discomfort.
Tubal Health
The only way to know if your tubes are causing infertility is to have them checked with imaging. The most serious blockages of the tube occur near the ovary, known as distal tubal occlusion. In those cases, there may be a condition known as hydrosalpinx, where a toxin is secreted into the uterus, which can interfere with implantation of the embryo causing IVF to be less successful. Therefore, even a couple who has, for example, known male factor infertility, should not skip checking the woman’s tubes. If her tubes were blocked by an unknown infection in her past and she has a hydrosalpinx condition, then she would not be able to conceive even with IVF. These hydrosalphinges should be surgically removed by an expert laparoscopic surgeon.
The hysterosalpingogram (HSG) and the FemVue tests are the x-ray and ultrasound-based methods to diagnose the anatomy of the uterus and the fallopian tubes. There are some individuals who may be at such low risk for tubal lockage, that the HSG is omitted.
Hysterosalpingogram (HSG)
If tubal blockage is suspected, using x-ray and fluoroscopy, a special dye, injected into the uterus, travels into the fallopian tubes. X-rays are used to determine if the tubes are open, and if there is a blockage, to determine the site of the blockage. Proximal tubal occlusion, when the tubes do not show up at all on the imaging may be due to tubal spasm or to disease, indicating actual blockage. This is an uncomfortable test done around day 7 to 12 of a woman’s menstrual cycle and can involve some discomfort, vaginal spotting, or bleeding afterwards.
FemVue Test
The FemVue test involves injecting a saline solution with air bubbles into the uterus to view the fallopian tubes. Using ultrasound, the bubbles shine and outline the tubes so that your doctor can determine if your tubes are open or blocked.
Laparoscopy
Laparoscopy involves a surgical procedure under anesthesia to look inside the abdomen. A telescope is introduced through a small incision in the umbilical area. With other instruments, the tubes and ovaries can be moved around and checked for physical problems such as endometriosis or scar tissue. Endometriosis particularly can be successfully treated with the laparoscope.
Can I predict fertility before I see a doctor?
The time-honored basal body temperature is a way of determining if a woman ovulates. However, it is not a great way to predict the most fertile time to conceive since the temperature rises the day after ovulation occurs. This information is only useful in retrospect if you used timed intercourse appropriately and did not get pregnant.
Cervical Mucus Observation
Cervical mucus observation is still a reliable, although not often discussed, way of determining the days when ovulation is approaching. Cervical mucus is detectable at the entrance to the vagina. The mucus becomes stretchy and thin like an egg white during ovulation. The observation of this change over three months can be helpful in determining the fertile window. This might be particularly important if cycle lengths vary.
Home Ovulation Test Kits
The home ovulation test kits available in drug stores are highly reliable in picking up the LH hormone surge which predicts ovulation, usually occurring on day 14 in a 28-day cycle after a menstrual period start. If, after following the directions carefully, there is a positive surge for a couple of months in a row, it is sufficient information to reassure everyone that ovulation is occurring.

Fertility Apps
Fertility apps are a modern-day version of the calendar method of determining the fertile period. If you record 3 or 4 cycles and note that ovulation is highly probable 14 or 15 days prior to the starting date of the next period, you could use this information to make an educated guess as to what will happen the next month.
Blood Test
If there is any question about ovulation then there is a blood test of progesterone, which can easily be done. If your periods are regular, then it can be done around day 21 of your cycle. Your doctor may have to help you determine the best day to do this test if your periods are irregular. However, since the history is so reliable, infertility specialists skip this test most of the time.

















